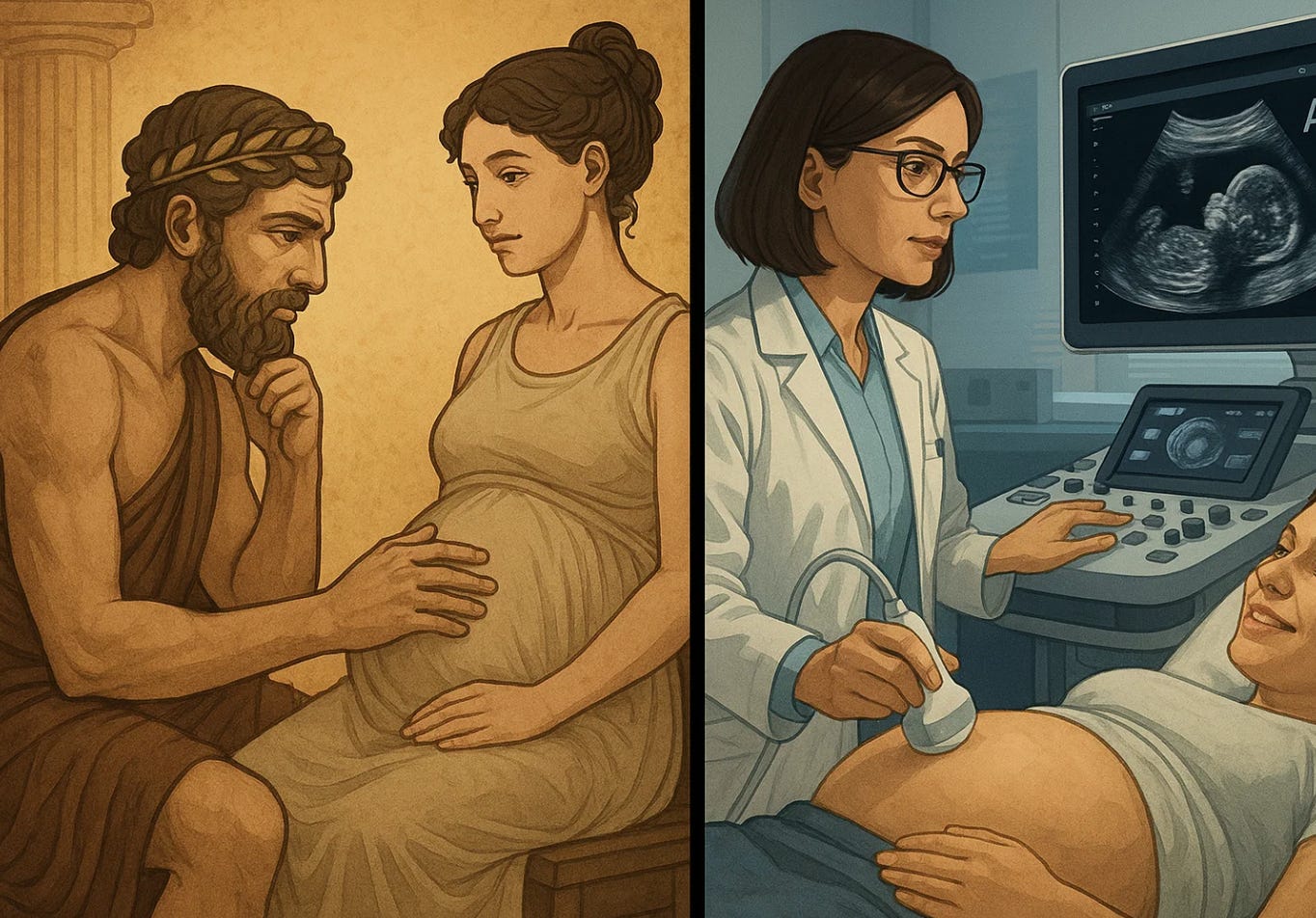
From Hippocrates to Artificial Intelligence: The Changing Face of Obstetrics in the New Time of A.I.
The art of obstetrics began with observation and judgment. A.I. is teaching us how to reclaim both—through data, discipline, and humility. The Prognosis — Forecasting where medicine, will go.
From the first recorded descriptions of pregnancy in Hippocratic texts to the predictive algorithms of the present, obstetrics has always stood at the edge of knowledge and uncertainty. It is one of medicine’s oldest arts, and perhaps now its most technologically transformed. Hippocrates relied on observation—changes in the eyes, breasts, or pulse—to infer pregnancy. Today, artificial intelligence can analyze ultrasound images, genomic patterns, and vital sign trajectories to anticipate complications weeks before symptoms appear. The constant across two and a half millennia is the same question: how can we see what is coming before it is too late?
The Hippocratic physician prized pattern recognition, not machines. He studied what nature revealed and sought to intervene only when necessary. In that sense, A.I. may be closer to Hippocrates than it appears. It thrives on pattern recognition—absorbing thousands of pregnancies, thousands of labors, thousands of outcomes—and finding meaning within the noise. What the ancients did by intuition, algorithms now do by computation. The challenge for today’s obstetrician is not whether to use A.I., but how to use it wisely, without surrendering professional judgment to the machine.
In the modern delivery suite, A.I. already assists with ultrasound interpretation, fetal heart rate pattern analysis, preeclampsia prediction, and postpartum hemorrhage risk assessment. These systems outperform humans at speed and consistency, yet they depend entirely on the quality of the data and the integrity of the clinician overseeing them. The ethical responsibility remains unchanged from Hippocrates’ era: to use knowledge for benefit and never for harm. What has changed is the scale—an error in an algorithm can affect thousands of patients before it is detected. In this new age, beneficence must include vigilance.
The parallel between the Hippocratic Oath and A.I. ethics is striking. Both rest on restraint and accountability. Hippocrates warned against hubris—against pretending to know what one does not. A.I. systems, by contrast, often speak with misplaced confidence. A well-trained model can sound certain while being wrong. For obstetrics, this is a dangerous illusion. When a clinician mistakes confidence for accuracy, lives can be lost. The moral task, then, is not to humanize A.I., but to professionalize its use—to ensure that humility remains part of its deployment.
Technology has always reshaped childbirth. The obstetric forceps, the fetal stethoscope, the electronic monitor, and now predictive analytics—each promised greater safety, and each raised new ethical questions. A.I. brings the same duality: its ability to detect subtle risk patterns in fetal distress or postpartum hemorrhage could save countless lives, yet its use in triage and risk scoring could also reinforce bias if training data are unrepresentative. Hippocrates’ dictum “first, do no harm” must now include protecting patients from algorithmic harm—harm that hides behind code.
Equity is the defining test of this transformation. A.I. systems trained on predominantly Western hospital data may underperform in low-resource or racially diverse settings. The same models that promise precision can inadvertently widen disparities in maternal mortality, already highest among Black and Indigenous women. The remedy is not rejection but correction: inclusive datasets, transparent validation, and ethical oversight built into development. To be truly Hippocratic, A.I. in obstetrics must learn from every woman, not just those whose data are easiest to collect.
And yet, the promise is extraordinary. A.I. can now integrate continuous home blood pressure readings, wearable data, and laboratory results to detect early preeclampsia; it can summarize charts, track postpartum recovery, and assist in counseling patients with fetal anomalies. Properly used, it can extend—not replace—the physician’s capacity for vigilance and compassion. Where Hippocrates observed with the eyes, A.I. observes with the cloud. The physician remains the interpreter, translating numbers into meaning.
The new face of obstetrics will not belong to a robot or a program. It will belong to the clinician who knows how to use these tools ethically, the educator who teaches discernment alongside data literacy, and the patient who demands transparency and respect. The Hippocratic ideal survives, reframed: the wise use of knowledge in service of life.
A.I. does not end the story of obstetrics. It brings it full circle—from ancient observation to digital empathy, from handwritten notes to predictive insight. What began as an art of watching and listening now returns to that same foundation, amplified by algorithms but still anchored in human judgment. The physician of the future will need the mind of a scientist, the humility of a humanist, and perhaps a little of Hippocrates’ patience.